Abstract
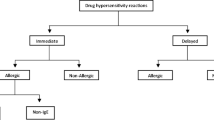
Acute hypersensitivity reactions (HSRs) are an unpredictable and potentially catastrophic complication of treatment with chemotherapeutic agents. Reactions may affect any organ system in the body and range widely in severity from mild pruritus to systemic anaphylaxis. Certain classes of chemotherapeutic agents, such as the taxanes, platinum compounds, asparaginases, and epipodophyllotoxins are commonly associated with HSRs. The clinical characteristics of these high risk agents with respect to HSRs are discussed in this review.
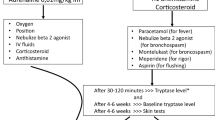
Protocols to prevent or reduce the severity of these reactions have been developed, but despite these attempts, HSRs will still happen. Should a reaction occur, it is imperative that it be recognised quickly in order to minimise exposure to the inciting agent and implement appropriate therapeutic and supportive measures. When a patient becomes sensitised to a chemotherapeutic agent, avoidance of re-exposure is the mainstay of future prevention. For sensitised patients who have derived clinically meaningful benefit from a particular agent, however, continuation of treatment with the agent is desirable. Options may include attempting a trial of desensitisation or treatment with a related compound. Virtually all patients demonstrating HSRs to paclitaxel and docetaxel are able to successfully tolerate re-treatment following discontinuation and administration of diphenhydramine and hydrocortisone. Re-treatment has generally been less successful with platinum compounds, with recurrent HSRs occurring in up to 50% of patients following desensitisation protocols. Patients sensitised to asparaginase are often able to tolerate the alternative preparations, Erwinia carotovora asparaginase or polyethylene glycol-modified Escherichia coli asparaginase. There is very little experience with re-treatment following sensitisation to the epipodophyllotoxins. As re-treatment may have serious consequences, careful consideration of the risks and benefits of these strategies is imperative when deciding among these options.







Similar content being viewed by others
References
Greenberger PA, Patterson R, Simon R, et al. Pretreatment of high-risk patients requiring radiographic contrast media studies. J Allergy Clin Immunol 1981; 67: 185–7
Trudeau ME, Eisenhauer EA, Higgins BP, et al. Docetaxel in patients with metastatic breast cancer: a Phase II study of the National Cancer Institute of Canada-Clinical Trials Group. J Clin Oncol 1996; 14: 422–8
Verweij J, Clavel M, Chevalier B. Paclitaxel (Taxol) and docetaxel (Taxotere): not simply two of a kind. Ann Oncol 1994; 5: 495–505
Eisenhauer EA, ten Bokkel Huinink WW, Swenerton KD, et al. European-Canadian randomized trial of paclitaxel in relapsed ovarian cancer: high-dose versus low-dose and long versus short infusion. J Clin Oncol 1994; 12: 2654–66
Weiss RB, Donehower RC, Wiernik PH, et al. Hypersensitivity reactions from Taxol. J Clin Oncol 1990; 8: 1263–8
Markman M, Kennedy A, Webster K, et al. Paclitaxel-associated hypersensitivity reactions: experience of the gynecologic oncology program of the Cleveland Clinic Cancer Center. J Clin Oncol 2000; 18: 102–5
Akerly W, Glantz M, Choy H, et al. Phase I trial of weekly paclitaxel in advances lung cancer. J Clin Oncol 1998; 16: 153–8
Burris H. Weekly schedules of docetaxel. Semin Oncol 1998; 25Suppl. 13: 21–3
Tomiak E, Piccart MJ, Kerger J, et al. Phase I study of docetaxel administered as a 1-hous intravenous infusion on a weekly basis. J Clin Oncol 1994; 12: 1458–67
Trivedi c, Redman B, Flaherty LE, et al. Weekly 1-hour infusion of paclitaxel: clinical feasibility and efficacy in patients with hormone-refractory prostate carcinoma. Cancer 2000; 89: 431–6
Lorenz W, Reimann HJ, Schmal A, et al. Histamine release in dogs by Cremophor EL and its derivatives: oxethylated oleic acid is the most effective constituent. Agents Actions 1977; 7: 63–7
Essayan DM, Kagey-Sobotka A, Colarusso PJ, et al. Successful parenteral desensitization for paclitaxel. J Allergy Clin Immunol 1996; 97: 42–6
McGuire WP, Hoskins WJ, Brady MF, et al. Cyclophosphamide and cisplatin compared with paclitaxel and cisplatin in patients with stage III and stage IV ovarian cancer. N Engl J Med 1996; 334: 1–6
Markman M, Kennedy A, Webster K, et al. Simplified regimen for the prevention of paclitaxel-associated hypersensitivity reactions. J Clin Oncol 1997; 15(12): 3517
Bookman MA, Kloth DD, Kover PE, et al. Intravenous prophylaxis for paclitaxel-related hypersensitivity reactions. Semin Oncol 1997; 24(6 Suppl. 19): S19–13–S19–15
Langer CJ, Leighton JC, Comis RL, et al. Paclitaxel and carboplatin in combination in the treatment of advanced nonsmall cell lung cancer: a phase II toxicity, response, and survival analysis. J Clin Oncol 1995; 13: 1860–70
Trudeau ME, Eisenhauer EA, Higgins BP, et al. Docetaxel in patients with metastatic breast cancer: a phase II study of the National Cancer Institute of Canada-Clinical Trials Group. J Clin Oncol 1996; 14: 422–8
Verweij J, Clavel M, Chevalier B. Paclitaxel (Taxol) and docetaxel (Taxotere): not simply two of a kind. Ann Oncol 1994; 5(6): 495–505
Piccart MJ, Klijn J, Paridaens R, et al. Corticosteroids significantly delay the onset of docetaxel-induced fluid retention: final results of a randomized study of the European Organization for Research and Treatment of Cancer Investigational Drug Branch for Breast Cancer. J Clin Oncol 1997; 15(9): 3149–55
Takanow R. Docetaxel: a taxoid for the treatment of metastatic breast cancer. Am Soc Health Syst Pharm 1998; 55(17): 1777–91
Wanders J, Schrijvers D, Bruntsch U, et al. The EORTC-ECTG experience with acute hypersensitivity reactions in Taxotere studies. Proc ASOC 1993; 12: 73
Schrijvers D, Wanders J, Dirix L, et al. Coping with toxicities of docetaxel. Ann Oncol 1993; 4: 610–1
Lokich J. Phase I clinical trial of weekly combined paclitaxel plus docetaxel in patients with solid tumors. Cancer 2000; 89: 2309–14
Adachi I, Watanabe T, Takashima S, et al. A late phase II study of docetaxel in patients with advanced or recurrent breast cancer. Br J Cancer 1996; 73: 210–6
Pazdur R, Lassere Y, Soh LT, et al. Phase II trial of docetaxel in metastatic colorectal carcinoma. Ann Oncol 1994; 11945: 468
Lokich J, Anderson N. Paclitaxel hypersensitivity reactions: a role for docetaxel substitution. Ann Oncol 1998; 9: 573–4
Weiss ME, Adkinson NF. Immediate hypersensitivity reactions to penicillin and related antibiotics. Clin Allergy 1988; 18: 515–40
Stark BJ, Earl HS, Gross GN, et al. Acute and chronic desensitization of penicillin-allergic patients using oral penicillin. J All Clin Immunol 1987; 79: 523–32
Cleare MJ, Highes EG, Jacoby B, et al. Immediate (type I) allergic responses to platinum compounds. Clin Allergy 1976; 6: 183–95
Shukunami K, Kuorkawa T, Kawakami Y, et al. Hypersensitivity reactions to intraperitoneal administration of carboplatin in ovarian cancer: the first report of a case. Gyn Oncol 1999; 72(3): 431–2
Blumenreich MS, Needles B, Yagoda A, et al. Intravesical cisplatin for superficial bladder tumors. Cancer 1982; 50: 863–5
Denis L. Anaphylactoid reactions to repeated intravesical installation with cisplatin. Lancet 1983; I: 1378–9
Markman M, Kennedy A, Webster K, et al. Clinical features of hypersensitivity reactions to carboplatin. J Clin Oncol 1999; 17: 1141–5
Weiss RB. Hypersensitivity reactions. Semin Oncol 1992; 19(5): 458–77
Zweizig S, Roman LD, Muderspach LI. Death from anaphylaxis to cisplatin: a case report. Gynecol Oncol 1994; 53(1): 121–2
Saunders MP, Denton CP, O’Brien ME, et al. Hypersensitivity reactions to cisplatin and carboplatin: a report on six cases. Ann Oncol 1992; 3(7): 574–6
Cromwell O, Papys J, Parish WE, et al. Specific IgE antibodies to platinum salts in sensitized workers. Clin Allergy 1979; 9: 109–17
Zanotti KM, Kennedy AW, Belinson JL, et al. A simplified skin testing protocol for predicting hypersensitivity to carboplatin chemotherapy [abstract]. Gynecol Oncol 2000; 76(2): 241
Shlebak AA, Clark PI, Green JA. Hypersensitivity and cross-reactivity to cisplatin and analogues. Cancer Chemother Pharmacol 1995; 35(4): 349–51
Weidmann B, Mulleneisen N, Bojko P, et al. Hypersensitivity reactions to carboplatin: report of two patients, review of the literature, and discussion of diagnostic procedures and management. Cancer 1994; 73(8): 2218–22
Chang SM, Fryberger S, Crouse V, et al. Carboplatin hypersensitivity in children: a report of five patients with brain tumors. Cancer 1995; 75(5): 1171–5
Broome CB, Schiff RI, Friedman HS. Successful desensitization to carboplatin in patients with systemic hypersensitivity reactions. Med Pediatr Oncol 1996; 26(2): 105–10
Kook H, Kim HM, Choi SH, et al. Life-threatening carboplatin hypersensitivity during conditioning for autologous PBSC transplantation: successful rechallenge after desensitization. BMT 1998; 21(7): 727–9
Rose PG, Fusco N, Fluellen L, et al. Carboplatin hypersensitivity reactions in patients with ovarian and peritoneal carcinoma. Int J Gynecol Cancer 1998 8: 365–6
Billett AL, Carls A, Belber RD, et al. Allergic reactions to Erwinia asparaginase in children with acute lymphoblastic leukemia who had previous allergic reactions to Escherichia coli asparaginase. Cancer 1992; 70(1): 201–6
Evans WE, Tsiatis A, Rivera G, et al. Anaphylactoid reactions to Escherichia coli and Erwinia asparaginase in children with leukemia and lymphoma. Cancer 1982; 49: 1378–83
Nesbit ME, Chard R, Evans A, et al. Evaluations of intramuscular versus intravenous administration of L-asparaginase in childhood leukemia. Am J Pediatr Hematol Oncol 1979; 1: 9–13
Albo V, Miller D, Leiken S, et al. Toxicity experience with a second course of E. coli L-asparaginase therapy 3 years after induction course in children with acute lymphoblastic leukemia in continuous remission [abstract]. Proc Am Soc Clin Oncol 1983; 68
Spiegel RJ, Echelberger CK, Poplack DG. Delayed allergic reactions following intramuscular L-asparaginase. Med Pediatr Oncol 1980; 8(2): 123–5
Asselin BL. The three asparaginases. Comparative pharmacology and optimal use in childhood leukemia. Adv Exp Med Biol 1999; 457: 621–9
Woo MH, Hak LJ, Storm MC, et al. Hypersensitivity or development of antibodies to asparaginase does not impact treatment outcome of childhood acute lymphoblastic leukemia. J Clin Oncol 2000; 18(7): 1525–32
Larson RA, Fretzin MH, Dodge RK, et al. Hypersensitivity reactions to L-asparaginase do not impact on the remission duration of adults with acute lymphoblastic leukemia. Leukemia 1998; 12(5): 660–5
Korholz D, Wahn U, Jurgens H, et al. Allergic reactions in treatment with L-asparaginase. Significance of specific IgE antibodies Monatsschrift Kinderheilkunde 1990; 138(1): 23–5
Woo MH, Hak LJ, Storm MC, et al. Anti-asparaginase antibodies following E. coli asparaginase therapy in pediatric acute lymphoblastic leukemia. Leukemia 1998; 12(10): 1527–33
Capizzi RL, Bertino JR, Handschumacher RE. L-asparaginase. Annu Rev Med 1970; 21: 433–42
Land VH, Sutow WW, Fernbach DJ, et al. Toxicity of L-asparaginase in children with advanced leukemia. Cancer 1972; 40: 339–47
The United states Pharmacopeial Convention. USP dispensing information: Vol. I: drug information for the health care professional. Englewood (CO): Micromedex Inc., 2000
Muller HJ, Loning L, Horn A, et al. Pegylated asparaginase (Oncaspar) in children with acute lymphoblastic leukemia: drug monitoring in reinduction according to the ALL/NHLBFM 95 protocols. Br J Haematol 2000; 111(2): 379–84
Sikorska-Fic B, Makowska K, Rokicka-Milewska R. New possibilities of treatment with PEG-L-asparaginase in patients with acute lymphoblastic leukemia sensitized to L-asparaginase E. coli and erwinase. Wiadomosci Lekarskie 1998; 51Suppl. 4: 233–6
Bonno M, Kawasaki H, Hori H, et al. Rapid desensitization for L-asparaginase hypersensitivity. J Allergy Clin Immunol 1998; 101(4 Pt 1): 571–2
Rodriguez T, Baumgarten E, Fengler R, et al. Long-term infusion of L-asparaginase—an alternative to intramuscular injection? Klin Padiatr 1995; 207(4): 207–10
O’Dwyer PJ, King SA, Fortner CL, et al. Hypersensitivity reactions to teniposide (VM-26): an analysis. J Clin Oncol 1986; 4(8): 1262–9
Kellie SJ, Crist WM, Pui C, et al. Hypersensitivity reactions to epiphodophyllotoxins in children with acute lymphoblastic leukemia. Cancer 1991; 67: 1070–5
Nolte H, Carstensen H, Hertz H. VM-26 (teniposide)-induced hypersensitivity and degranulation of basophils in children. Am J Pediatr Hematol Oncol 1988; 10(4): 308–12
Carstensen H, Nolte H, Hertz H. Teniposide-induced hypersensitivity reactions in children. Lancet 1989; II: 55
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zanotti, K.M., Markman, M. Prevention and Management of Antineoplastic-Induced Hypersensitivity Reactions. Drug-Safety 24, 767–779 (2001). https://doi.org/10.2165/00002018-200124100-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200124100-00005