Abstract
Cells deficient in the Brca1 and Brca2 genes have reduced capacity to repair DNA double-strand breaks by homologous recombination and consequently are hypersensitive to DNA-damaging agents, including cisplatin and poly(ADP-ribose) polymerase (PARP) inhibitors. Here we show that loss of the MLL3/4 complex protein, PTIP, protects Brca1/2-deficient cells from DNA damage and rescues the lethality of Brca2-deficient embryonic stem cells. However, PTIP deficiency does not restore homologous recombination activity at double-strand breaks. Instead, its absence inhibits the recruitment of the MRE11 nuclease to stalled replication forks, which in turn protects nascent DNA strands from extensive degradation. More generally, acquisition of PARP inhibitors and cisplatin resistance is associated with replication fork protection in Brca2-deficient tumour cells that do not develop Brca2 reversion mutations. Disruption of multiple proteins, including PARP1 and CHD4, leads to the same end point of replication fork protection, highlighting the complexities by which tumour cells evade chemotherapeutic interventions and acquire drug resistance.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Lord, C. J. & Ashworth, A. Mechanisms of resistance to therapies targeting BRCA-mutant cancers. Nature Med. 19, 1381–1388 (2013)
Schlacher, K. et al. Double-strand break repair-independent role for BRCA2 in blocking stalled replication fork degradation by MRE11. Cell 145, 529–542 (2011)
Schlacher, K., Wu, H. & Jasin, M. A distinct replication fork protection pathway connects Fanconi anemia tumor suppressors to RAD51-BRCA1/2. Cancer Cell 22, 106–116 (2012)
Ying, S., Hamdy, F. C. & Helleday, T. Mre11-dependent degradation of stalled DNA replication forks is prevented by BRCA2 and PARP1. Cancer Res. 72, 2814–2821 (2012)
Pathania, S. et al. BRCA1 haploinsufficiency for replication stress suppression in primary cells. Nature Commun . 5, 5496 (2014)
Pathania, S. et al. BRCA1 is required for postreplication repair after UV-induced DNA damage. Mol. Cell 44, 235–251 (2011)
Bunting, S. F. et al. BRCA1 functions independently of homologous recombination in DNA interstrand crosslink repair. Mol. Cell 46, 125–135 (2012)
Bunting, S. F. et al. 53BP1 inhibits homologous recombination in Brca1-deficient cells by blocking resection of DNA breaks. Cell 141, 243–254 (2010)
Bouwman, P. et al. 53BP1 loss rescues BRCA1 deficiency and is associated with triple-negative and BRCA-mutated breast cancers. Nature Struct. Mol. Biol . 17, 688–695 (2010)
Callen, E. et al. 53BP1 mediates productive and mutagenic DNA repair through distinct phosphoprotein interactions. Cell 153, 1266–1280 (2013)
Chapman, J. R. et al. RIF1 is essential for 53BP1-dependent nonhomologous end joining and suppression of DNA double-strand break resection. Mol. Cell 49, 858–871 (2013)
Escribano-Díaz, C. et al. A cell cycle-dependent regulatory circuit composed of 53BP1-RIF1 and BRCA1-CtIP controls DNA repair pathway choice. Mol. Cell 49, 872–883 (2013)
Feng, L., Fong, K. W., Wang, J., Wang, W. & Chen, J. RIF1 counteracts BRCA1-mediated end resection during DNA repair. J. Biol. Chem. 288, 11135–11143 (2013)
Di Virgilio, M. et al. Rif1 prevents resection of DNA breaks and promotes immunoglobulin class switching. Science 339, 711–715 (2013)
Zimmermann, M., Lottersberger, F., Buonomo, S. B., Sfeir, A. & de Lange, T. 53BP1 regulates DSB repair using Rif1 to control 5′ end resection. Science 339, 700–704 (2013)
Hashimoto, Y., Ray Chaudhuri, A., Lopes, M. & Costanzo, V. Rad51 protects nascent DNA from Mre11-dependent degradation and promotes continuous DNA synthesis. Nature Struct. Mol. Biol . 17, 1305–1311 (2010)
Kuznetsov, S. G., Liu, P. & Sharan, S. K. Mouse embryonic stem cell-based functional assay to evaluate mutations in BRCA2. Nature Med. 14, 875–881 (2008)
Willis, N. A. et al. BRCA1 controls homologous recombination at Tus/Ter-stalled mammalian replication forks. Nature 510, 556–559 (2014)
Sonoda, E. et al. Sister chromatid exchanges are mediated by homologous recombination in vertebrate cells. Mol. Cell. Biol. 19, 5166–5169 (1999)
Toledo, L. I. et al. A cell-based screen identifies ATR inhibitors with synthetic lethal properties for cancer-associated mutations. Nature Struct. Mol. Biol . 18, 721–727 (2011)
Mirzoeva, O. K. & Petrini, J. H. DNA replication-dependent nuclear dynamics of the Mre11 complex. Mol. Cancer Res. 1, 207–218 (2003)
Dungrawala, H. et al. The replication checkpoint prevents two types of fork collapse without regulating replisome stability. Mol. Cell 59, 998–1010 (2015)
Cho, Y. W. et al. PTIP associates with MLL3- and MLL4-containing histone H3 lysine 4 methyltransferase complex. J. Biol. Chem. 282, 20395–20406 (2007)
Patel, S. R., Kim, D., Levitan, I. & Dressler, G. R. The BRCT-domain containing protein PTIP links PAX2 to a histone H3, lysine 4 methyltransferase complex. Dev. Cell 13, 580–592 (2007)
Gong, Z., Cho, Y. W., Kim, J. E., Ge, K. & Chen, J. Accumulation of Pax2 transactivation domain interaction protein (PTIP) at sites of DNA breaks via RNF8-dependent pathway is required for cell survival after DNA damage. J. Biol. Chem. 284, 7284–7293 (2009)
Starnes, L. M. et al. A PTIP-PA1 subcomplex promotes transcription for IgH class-switching independently from the associated MLL3/MLL4 methyltransferase complex. Genes Dev 30, 149–163 (2016)
Buonomo, S. B., Wu, Y., Ferguson, D. & de Lange, T. Mammalian Rif1 contributes to replication stress survival and homology-directed repair. J. Cell Biol. 187, 385–398 (2009)
Guillemette, S. et al. Resistance to therapy in BRCA2 mutant cells due to loss of the nucleosome remodeling factor CHD4. Genes Dev. 29, 489–494 (2015)
Bryant, H. E. et al. PARP is activated at stalled forks to mediate Mre11-dependent replication restart and recombination. EMBO J. 28, 2601–2615 (2009)
Ding, X. et al. Synthetic viability by BRCA2 and PARP1/ARTD1 deficiencies. Nature Commun. http://dx.doi.org/10.1038/ncomms12425 (2016)
Bryant, H. E. et al. Specific killing of BRCA2-deficient tumours with inhibitors of poly(ADP-ribose) polymerase. Nature 434, 913–917 (2005)
Farmer, H. et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature 434, 917–921 (2005)
Jonkers, J. et al. Synergistic tumor suppressor activity of BRCA2 and p53 in a conditional mouse model for breast cancer. Nature Genet. 29, 418–425 (2001)
Chen, H. et al. Sae2 promotes DNA damage resistance by removing the Mre11-Rad50-Xrs2 complex from DNA and attenuating Rad53 signaling. Proc. Natl Acad. Sci. USA 112, E1880–E1887 (2015)
Puddu, F. et al. Synthetic viability genomic screening defines Sae2 function in DNA repair. EMBO J. 34, 1509–1522 (2015)
Moynahan, M. E., Pierce, A. J. & Jasin, M. BRCA2 is required for homology-directed repair of chromosomal breaks. Mol. Cell 7, 263–272 (2001)
Ward, I. M. et al. 53BP1 is required for class switch recombination. J. Cell Biol. 165, 459–464 (2004)
Lee, J. E. et al. H3K4 mono- and di-methyltransferase MLL4 is required for enhancer activation during cell differentiation. eLife 2, e01503 (2013)
Cho, Y. W. et al. Histone methylation regulator PTIP is required for PPARγ and C/EBPα expression and adipogenesis. Cell Metab. 10, 27–39 (2009)
Liu, W. et al. A selective small molecule DNA2 inhibitor for sensitization of human cancer cells to chemotherapy. EBioMedicine 6, 73–86 (2016)
Pierce, A. J., Johnson, R. D., Thompson, L. H. & Jasin, M. XRCC3 promotes homology-directed repair of DNA damage in mammalian cells. Genes Dev. 13, 2633–2638 (1999)
Ray Chaudhuri, A. et al. Topoisomerase I poisoning results in PARP-mediated replication fork reversal. Nature Struct. Mol. Biol . 19, 417–423 (2012)
Rottenberg, S. et al. Selective induction of chemotherapy resistance of mammary tumors in a conditional mouse model for hereditary breast cancer. Proc. Natl Acad. Sci. USA 104, 12117–12122 (2007)
Xu, G. et al. REV7 counteracts DNA double-strand break resection and affects PARP inhibition. Nature 521, 541–544 (2015)
Acknowledgements
We thank A. Bhandoola for discussions; K. Wolcott for flow cytometry; R. Faryabi for help with statistical analysis; T. de Lange for Rif1f/f mice, J. Tainer for PFM39, R. Brosh for WRNi and J. Petrini for Mre11 antibodies. This work was supported by the Intramural Research Program of the National Institutes of Health (NIH), the National Cancer Institute and the Center for Cancer Research, and by a Department of Defense grant to A.N. (BCRP DOD Idea Expansion Award, grant 11557134), and the Netherlands Organization for Scientific Research, the Dutch Cancer Society and the Swiss National Science Foundation to S.V. A.R.C. was supported by a Prospective Researcher Award from Swiss National Science Foundation (PBZHP3_147302) and Human Frontier Science Program Long-Term Fellowship (LT000393/2013). S.C. was supported by NIH grant R01 CA176166-01A1; B.S. was supported by NIH grant R01CA085344; and J.A.D. was supported by a grant to the Center for Protein Research from the Novo Nordisk Foundation (NNF14CC0001).
Author information
Authors and Affiliations
Contributions
A.R.C., E.C., S.S. and A.N. conceived and planned the study. A.R.C., E.C. and X.D. designed, performed experiments and analysed data on B cells, MEFS and ESCs. E.G. and A.A.D. generated and performed experiments on PARPi-resistant tumours. J.J. and S.R. supervised the studies on PARPi-resistant tumours. N.W., A.D. and S.J. helped with experimentation. J.E.L. and K.G. generated Mll4- and Mll4-SET-deficient mice. L.S. and J.D. generated PTIP deletion constructs. B.S. provided reagents for experiments. D.C. provided advice on performing iPOND experiments and supervised iPOND mass spectrometry. J.C., N.P. and S.C. provided shCHD4 PEO1 cells and performed immunofluorescence experiments. P.K. analysed TCGA databases. V.F. and O.F.C. performed high-throughput image analysis of MRE11. S.S. supervised the ESC studies. A.R.C., E.C. and A.N. wrote the manuscript and all authors reviewed it.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Additional information
Source tumour measurement data are provided in Supplementary Information.
Extended data figures and tables
Extended Data Figure 1 Fork degradation in Brca-deficient B lymphocytes is mediated by MRE11 exonuclease activity.
a, b, Ratio of IdU versus CldU upon HU treatment in WT, Brca1−/− (a) and WT, Brca2−/− (b) B lymphocytes with or without mirin pre-treatment. Numbers in red indicate the mean ± s.d. for each sample (**P ≤ 0.05, ***P ≤ 0.001, ****P ≤ 0.0001, Mann–Whitney test). One hundred and twenty-five replication forks were analysed for each genotype. c, Ratio of IdU versus CldU upon HU treatment in Brca2−/− B lymphocytes with or without mirin, PFM39 (MRE11 exonuclease inhibitor), PC5 (DNA2 inhibitor) or WRNi pre-treatment. Numbers in red indicate the mean ± s.d. for each sample (**P ≤ 0.05, ****P ≤ 0.0001, Mann–Whitney test). One hundred and twenty-five replication forks were analysed for each genotype.
Extended Data Figure 2 Replication fork progression rates and DSBs in B lymphocytes.
a, Quantificative PCR analysis for Brca1, Brca2, Ptip and Rif1 gene deletions in WT, Brca1−/−, Brca1−/− Rif1−/−, Brca1−/−Ptip−/−, Brca2−/− and Brca2−/− Ptip−/− primary B lymphocytes after infection with CRE. b, PFGE analysis for detection of DSBs in WT, Brca2−/− and Brca2−/− Ptip−/− B lymphocytes treated with or without 4 mM HU for 3 h. Positive control for DSBs includes treatment of 15 Gy irradiation and HU +ATRi treatment for 3 h. Quantification of fold change in DSBs across genotypes relative to non-treated WT is plotted on the right. c–f, Replication fork progression rates, measured by tract lengths in micrometres, of CldU (red) and IdU (green) in WT, Brca1−/−, Brca1−/− 53Bp1−/−, Rif1−/−, Brca1−/− Rif1−/−, Ptip−/−, Brca1−/− Ptip−/−, Brca2−/− and Brca2−/− Ptip−/− primary B lymphocytes. Samples were not treated with HU. Numbers in red indicate the mean ± s.d. for each sample. One hundred and twenty-five replication forks were analysed for each genotype.
Extended Data Figure 3 Loss of PTIP rescues fork progression and restart defects in Brca2-deficient B lymphocytes but does not affect RAD51 IRIF.
a, Genomic instability measured in metaphase spreads from B lymphocytes derived from WT, Brca1−/−, Rif1−/−, Brca1−/−Rif1−/− mice treated for 6 h with 10 mM HU (*P ≤ 0.05, unpaired t-test). Fifty metaphases were analysed per condition. Experiments were repeated three times. b, Genomic instability measured in metaphase spreads from B lymphocytes derived from WT, Brca2−/−, Ptip−/−, Brca2−/−Ptip−/− mice treated for 6 h with 10 mM HU (*P ≤ 0.05, unpaired t-test). Fifty metaphases were analysed per condition. Experiments were repeated three times. c, Fork progression in B lymphocytes derived from WT, Brca2−/−, Ptip−/−, Brca2−/−Ptip−/− mice treated for 1 h with 0.2 mM HU. The y axis represents the tract lengths in micrometres. Numbers in red indicate the mean ± s.d. for each sample (****P ≤ 0.0001, Mann–Whitney test). One hundred and fifty replication forks were analysed for each genotype. d, Percentage of restarted replication forks in WT, Brca2−/−, Ptip−/−, Brca2−/−Ptip−/− B cells treated for 1 h with 1 mM HU followed by 90 min recovery. Two hundred replication forks were analysed for each genotype. e, Tract lengths of restarted replication forks in WT, Brca2−/−, Ptip−/−, Brca2−/−Ptip−/− B cells treated for 1 h with 1 mM HU followed by 90 min recovery. The y axis represents the tract lengths in micrometres. Numbers in red indicate the mean ± s.d. for each sample (NS, not significant, ****P ≤ 0.0001, Mann–Whitney test). One hundred and fifty replication forks were analysed for each genotype. f, Western blot analysis for RAD51 levels in WT, Ptip−/−, Brca2−/− and Brca2−/−Ptip−/− B cell extracts. Tubulin was used as loading control. g, Quantification of RAD51 foci formation in WT, Brca2−/− and Brca2−/−Ptip−/− B cells upon treatment with 5 and 10 Gy irradiation and recovery for 2, 4 and 6 h (n = 150 cells analysed).
Extended Data Figure 4 Depletion of PTIP rescues the lethality of Brca2-deficient ESCs.
a, Western blot analysis for PTIP levels in WT and two different clones of Brca2−/− ESCs electroporated with shPtip. b, Southern blot analysis for determination of Brca2 deletion in surviving clones electroporated with shPtip. Probes distinguishing the Brca2-flox allele (4.8 kb) (upper band) and Brca2 KO allele (2.2 kb) (lower band) were used. *Surviving ESC clones with Brca2 deletion and simultaneous downregulation of PTIP (12/96 Brca2-deleted colonies were found with shPtip1 and 3/60 colonies were found with shPtip2). Genotyping was confirmed by PCR (Fig. 2b). c, Top, representative FACS profiles of WT and Brca2−/−/shPtip ESCs electroporated with either pDR–GFP plasmid only (control) or pDRGFP and I-SceI expressing vector for 48 h. Gene conversion of the pDR–GFP construct by HR is determined by the percentage of GFP-positive cells (FL1, green-detection filter; FL2, red-detection filter). Bottom, quantification of the percentage of GFP-positive cells in WT and Brca2−/−/shPtip ESCs across three independent experiments. NS, not significant, *P ≤ 0. 05, unpaired t-test. d, Sister chromatid exchange (SCE) analysis in WT and Brca2Y3308X hypomorphic ESCs. Twenty metaphases were analysed per condition; experiments were repeated three times. e, WT and Brca2Y3308X hypomorphic ESCs were preincubated with mirin, EdU-labelled for 15 min and treated with 4 mM HU for 2 h. Proteins associated with replication forks were isolated by iPOND and detected by western blotting with the indicated antibodies. f, SCEs in WT, Brca2−/− and Brca2−/− Ptip−/− B cells either untreated or treated overnight with 1 μM PARPi or with 0.5 μM cisplatin (NS, not significant, *P ≤ 0.05, **P ≤ 0.001, unpaired t-test). Twenty metaphases were analysed per condition; experiments were repeated three times.
Extended Data Figure 5 PTIP localizes to sites to DNA replication independently of DSBs.
a, WT and 53Bp1−/− MEFs were retrovirally infected with a GFP-tagged PTIP construct. Cells were then irradiated with 10 Gy and allowed to recover. Co-localization of γ-H2AX (red) and PTIP (green) was assessed. Adjoining graph quantifies the percentage of cells with γ-H2AX foci co-localizing with PTIP upon irradiation (n = 150 cells analysed). Experiments were repeated three times. b, Western Blot analysis for endogenous and overexpressed PTIP levels in WT and 53Bp1−/− MEFs retrovirally infected with a GFP-tagged PTIP construct (GFP–PTIP). c, Quantification of the percentage of pan-nuclear γ-H2AX-positive cells with PTIP foci in WT and 53Bp1−/− MEFs upon treatment with HU (related to Fig. 3a) (n = 150 cells analysed). Experiments were repeated three times. d, Quantification of the percentage of cells with PTIP foci co-localizing with PCNA in WT and 53Bp1−/− MEFs in late S phase (related to Fig. 3b) (n = 150 cells analysed). Experiments were repeated three times. e, Representative immunofluorescence images of PCNA and 53BP1 co-staining in irradiated WT cells (10 Gy) or in late S-phase sites. White arrows indicate that the few 53BP1 foci observed in late S-phase cells do not co-localize with PCNA. (n = 50 cells analysed). Experiments were repeated three times. f, Representative immunofluorescence images of WT and Ptip−/− MEFs treated with 4 mM HU for 2 h and analysed for ssDNA (BrdU) and MRE11 co-localization. Bottom panels shows the quantification of BrdU-positive cells (left) and the percentage of MRE11 co-localization in BrdU-positive cells (right) upon HU treatment in WT and Ptip−/− MEFs. (n = 150 cells analysed). Experiments were repeated three times. g, Quantification of the percentage of cells with MRE11 foci co-localizing with γ-H2AX upon irradiation treatment (10 Gy) in WT and Ptip−/− MEFs (related to Fig. 3e) (n = 150 cells analysed). Experiments were repeated three times. h, Cell cycle profiles in WT and Ptip−/− MEFs as measured by the incorporation of EdU (y axis) vs. DAPI (x axis). i, iPOND coupled to SILAC Mass-Spectrometry analysis for PTIP, H4 and RPA enrichment at stalled forks in 293T cells upon 3 mM HU treatment for 10 min and 4 h (ref. 22). The y axes represent the relative abundance of the indicated proteins on a log2 scale.
Extended Data Figure 6 MLL3/4 promotes replication fork degradation in Brca2–deficient cells.
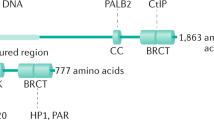
a, Top, schematic of the retroviral PTIP mutant constructs used to identify the domain of PTIP involved in driving replication fork degradation. Different BRCT domains in PTIP are numbered and Q represents the glutamine rich region between the second and the third BRCT domains. Bottom, ratio of IdU versus CldU upon HU treatment of Brca2−/− Ptip−/− B lymphocytes retrovirally infected with either EV, FL, W165R, W663R and Del BRCT 5-6 PTIP-mutant constructs and sorted for GFP or mCherry expression. Numbers in red indicate the mean ± s.d. for each sample (**P ≤ 0.01, ****P ≤ 0.0001, Mann–Whitney test). One hundred and twenty-five replication forks were analysed for each condition. b, WT and Mll3/4−/− MEFs were EdU-labelled for 15 min and treated with 4 mM HU for 4 h. Proteins associated with replication forks were isolated by iPOND and detected by western blotting with the indicated antibodies. c, Quantification of the percentage of cells with MRE11 foci co-localizing with PCNA in late S phase in WT and MLL3/4−/− MEFs (n = 150 cells analysed). Experiments were repeated three times. d–f, Ratio of IdU versus CldU upon HU treatment in WT, Brca1−/−, Brca2−/− Mll4−/−, Mll4-SET−/−, Brca1−/−Mll4−/−, Brca2−/−Mll4−/− and Brca1−/−Mll4-SET−/− B cells. Numbers in red indicate the mean ± s.d. for each sample (NS, not significant, ****P ≤ 0.0001, Mann–Whitney test). At least 125 replication forks were analysed for each genotype. g, Genomic instability measured in metaphase spreads from splenic B cells derived from WT, Brca2−/−, Mll4−/−, Brca2−/−Mll4−/− B cells treated overnight with 1 μM PARPi or with 0.5 μM cisplatin (**P ≤ 0.01, ***P ≤ 0.001, unpaired t-test). Fifty metaphases were analysed per condition. Experiments were repeated three times.
Extended Data Figure 7 Loss of RIF1 results in chromosomal instability.
a, Quantification of RAD51 foci formation in WT, Brca1−/− and Rif1−/− B cells. Cells were treated with 10 Gy and harvested 4 h after irradiation (NS, not significant, *P ≤ 0.05). At least 100 cells were analysed per condition; experiments were repeated three times. b, c, Genomic instability measured in metaphase spreads from splenic B cells derived from WT, Brca1−/− and Rif1−/− mice treated overnight with 1 μM PARPi (b) or with 0.5 μM cisplatin (c) (NS, not significant, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001, unpaired t-test). Fifty metaphases were analysed per condition; experiments were repeated three times.
Extended Data Figure 8 Multiple mutations can cause resistance to DNA-damaging agents in Brca-deficient cells.
a, b, Difference in progression-free survival (PFS) of BRCA2- and BRCA1-mutated ovarian serous adenocarcinoma patients with standard platinum-based regimens. Data were obtained from the TCGA project. Patients were separated into PTIP low- or high-expression on the basis of the 33rd percentile of PTIP expression z-scores. The difference between the PFS of PTIP-low versus PTIP-high was assessed by univariate log-rank P value (P < 0.072 and P < 0.032 in a and b, respectively). Analysis included 38 tumours with BRCA1 mutations and 34 tumours with BRCA2 mutations out of 316 high-grade serous ovarian cancers that underwent whole-exome sequencing. PFS curves for PTIP-low and PTIP-high expressing tumours were generated by the Kaplan–Meier method. All reported P values are two-sided. c, Western blot analysis for CHD4 and PTIP levels in PEO1 cells infected with shNSC and shCHD4. Tubulin was used as loading control. d, Cell cycle profiles in PEO1 cells infected with shNSC and shCHD4 as measured by the incorporation of EdU (y axis) versus DAPI (x axis). e, Immunostaining for MRE11 and PCNA in PEO1 cells infected with shNSC and shCHD4 upon treatment with 4 mM HU. Bottom, quantification for MRE11 recruitment upon HU treatment. At least 100 cells were analysed per condition; experiments were repeated three times. f, Western blot analysis for CHD4 and MRE11 levels in PEO1 cells infected with shNSC and shCHD4. Actin was used as loading control. g, Percentage of EdU-positive cells was analysed 20 h after Brca2−/− B cells were treated with mirin alone, mirin+PARPi or mirin+cisplatin (NS, not significant). EdU was pulsed for 20 min before FACS analysis. Experiments were repeated three times. h, Genomic instability measured in metaphase spreads from B cells derived from Brca2−/− mice pretreated with 25 μM mirin for 2 h followed by overnight treatment with 1 μM PARPi or 0.5 μM cisplatin (NS, not significant, *P ≤ 0.05, **P ≤ 0.001, unpaired t-test). Fifty metaphases were analysed per condition. Experiments were repeated three times. i, Quantification of RAD51 foci formation in WT, Brca1−/−, Parp1−/− and Brca1−/−Parp1−/− B cells treated with 10 Gy irradiation and harvested 4 h after treatment. At least 100 cells were analysed per condition; experiments were repeated three times.
Extended Data Figure 9 Brca2-deficient tumours acquire PARPi resistance without restoration of RAD51 foci formation.
a, Schematic depicting the conditional BRCA2 allele of the KB2P (K14CRE;Brca2f/f;p53f/f) spontaneous tumour model. b, Outline of the PARPi intervention study. A spontaneous BRCA2-/p53-deficient tumour was generated and re-transplated into syngeneic WT mice. When the tumours reached 200 mm3, they were treated either with vehicle or PARPi AZD2461. c, PARPi response curve of the KB2P tumour (relative tumour volume (rtv) versus days). The treatment for 28 consecutive days was started when the tumour reached 200 mm3 (rtv = 100%). In response to the treatment, the tumour shrank but eventually grew back. When it reached 100% relative tumour volume, the treatment was repeated (as indicated with red arrows) for another 28 days. This regime was continued until the tumour became resistant to PARPi (black arrow). d, The stability of acquired resistance of the KB2P tumour was confirmed by re-transplanting matched naive and resistant tumours and treating animals either with vehicle or AZD2461 (only one 28-day cycle). Kaplan–Meier survival curve indicates that resistant tumours did not respond to the AZD2461 treatment, while naive tumours exhibited high sensitivity, indicative of a stable genetic mechanism of resistance. e, f, Irradiation-induced RAD51 foci were detected by immunofluorescence in the KB2P donor: RAD51 foci formation was undetectable in naive and resistant tumours, suggesting that HR restoration is not an underlying mechanism of PARPi resistance. Spontaneous tumours from K14 Cre; p53f/f mice treated with irradiation were used as positive control for RAD51 foci. Unirradiated K14 Cre; p53f/f cells were used as a negative control. g, Replication fork progression rates measured by tract lengths in micrometres of CldU (red) and IdU (green) in PARPi-naive or PARPi-resistant tumours. Numbers in red indicate the mean ± s.d. for each sample. One hundred and twenty-five replication forks were analysed for each condition. h, Western blot analysis for PTIP and MRE11 levels in PARPi-naive or PARPi-resistant tumours. Tubulin was used as loading control.
Extended Data Figure 10 Brca2-deficient ESCs have higher levels of chromatin-bound MRE11.
a, Representative image of a Brca2 hypomorph mouse ESC (denoted Brca2Y3308X) showing MRE11 foci (red) in S phase (identified by PCNA foci (green)). DNA was stained with DAPI (blue). b, High-throughput microscopy analysis quantifying the overall levels of chromatin-bound MRE11 per individual nucleus in WT and Brca2Y3308X cells treated as indicated (a.u., arbitrary units).
Supplementary information
Supplementary Figure 1
This file contains the raw data (un-cropped blots and gels) from Figures 2b, 2e, 3f, and Extended Data Figures 2b, 3f, 4a, 4b, 4e, 5b, 6b, 8c, 8f, and 9h. (PDF 592 kb)
Supplementary Table 1
This table contains the measurements for tumor volume in the in naïve and resistant KB2P tumors. KB1P13 is the original tumor (PATHO 09 SRO 012), which was either vehicle treated (PATHO 09 SRO 238) or PARPi treated to induce resistance (PATHO 09 SRO 097). PROMASS indicates the barcode number of the mice. MDZ (MDZ 1383, MDZ 2630 and MDZ 2809) numbers are cryobank IDs corresponding to the original, naïve and resistant tumors respectively. (XLSX 36 kb)
Rights and permissions
About this article
Cite this article
Ray Chaudhuri, A., Callen, E., Ding, X. et al. Replication fork stability confers chemoresistance in BRCA-deficient cells. Nature 535, 382–387 (2016). https://doi.org/10.1038/nature18325
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nature18325
This article is cited by
-
Deubiquitinase USP7 stabilizes KDM5B and promotes tumor progression and cisplatin resistance in nasopharyngeal carcinoma through the ZBTB16/TOP2A axis
Cell Death & Differentiation (2024)
-
MBD1 protects replication fork stability by recruiting PARP1 and controlling transcription-replication conflicts
Cancer Gene Therapy (2024)
-
Meiotic protein SYCP2 confers resistance to DNA-damaging agents through R-loop-mediated DNA repair
Nature Communications (2024)
-
PARP Inhibitors in Breast Cancer: a Short Communication
Current Oncology Reports (2024)
-
Racial differences in RAD51 expression are regulated by miRNA-214-5P and its inhibition synergizes with olaparib in triple-negative breast cancer
Breast Cancer Research (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.