Abstract
Purpose
The aim of our study was to assess concordance of staging laparoscopy and cytoreductive surgery (CRS) peritoneal cancer index (PCI) when applying a two-step surgical protocol. We also aimed to evaluate the accuracy of diagnostic laparoscopy to triage patients for complete cytoreduction, and to define optimal time between staging laparoscopy and CRS.
Methods
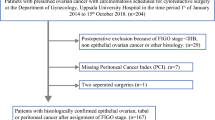
We designed a retrospective review of prospectively collected data from patients with advanced ovarian cancer who underwent a diagnostic laparoscopy followed by a CRS a few weeks later (two-step surgical protocol), from January 2010 to April 2019. Only patients selected for complete cytoreduction, and with available PCI score from both surgeries were included. PCI concordance was assessed using intraclass correlation coefficient (ICC).
Results
During the study period 543 patients underwent a laparoscopic staging for ovarian carcinomatosis. Among them, 43 patients fulfilled inclusion criteria. ICC between laparoscopic and laparotomic PCI was 0.54. After applying the linear regression equation: laparoscopic PCI + 0.2 x [days between surgeries] + 2, ICC increased to 0.79. Completeness cytoreduction score and laparoscopic PCI were significantly associated (OR 1.27, 95% CI 1.03–1.57, p = 0.03). AUC of laparoscopic PCI to predict complete cytoreduction was 0.90.
Conclusion
Concordance between laparoscopic PCI assessment and PCI score at the end of CRS is fair within a two-step surgical management. Laparoscopic assessment underestimates final PCI score by two points, and this difference increases with the delay between both surgeries. Diagnostic laparoscopy can adequately select patients for CRS, and optimal time to perform it is no more than 10 days after laparoscopy.
Similar content being viewed by others
Introduction
Complete cytoreduction without leaving macroscopic disease is the most important prognostic factor in advanced ovarian cancer [1, 2]. The gold standard treatment is the combination of cytoreductive surgery (CRS) with platinum and taxane-based chemotherapy [3]. In case of medically non-operable patients, or in case of low likelihood of achieving complete cytoreduction, neoadjuvant chemotherapy is performed [4]. To avoid unnecessary exploratory laparotomies and incomplete cytoreduction surgeries, and to decrease the delay to neoadjuvant chemotherapy due to surgical morbidity, it is necessary to assess the disease extent and to select which patients will undergo complete tumor resection. US NCCN current guidelines recommend diagnostic laparoscopy to evaluate whether maximal cytoreduction can be achieved in newly diagnosed ovarian cancer patients [5].
Staging laparoscopy has shown to be a minimally invasive tool able to properly drive the therapeutic choice between primary CRS and neoadjuvant chemotherapy [6,7,8]. To quickly select candidates for upfront surgery, and to decrease the delay to CRS or neoadjuvant chemotherapy, we offer patients a two-step surgical management protocol in which diagnostic laparoscopy is performed a few weeks prior to CRS.
Peritoneal cancer index (PCI) can be assessed either by laparoscopy or laparotomy. It describes the extent and anatomic distribution of peritoneal carcinomatosis, and it objectively quantifies the tumor burden [9]. Tentes et al. showed that peritoneal spread in advanced ovarian cancer could be assessed in detail using PCI, and that this score was a significant prognostic factor of survival [10]. Some studies have demonstrated a good reproducibility of PCI scores between senior and junior surgeons, and between laparoscopic and laparotomic assessment when performing a staging laparoscopy immediately before CRS [11]. However, laparoscopic and laparotomic PCI concordance has not yet been evaluated in a two-step surgical protocol.
The aim of our study was to assess the concordance between PCI of staging laparoscopy and CRS when applying a two-step surgical protocol. We also aimed to evaluate the accuracy of diagnostic laparoscopy to triage patients for complete cytoreduction, and to define optimal time between staging laparoscopy and CRS.
Methods
Patients and study design
We designed a retrospective review of prospectively collected data from patients with advanced epithelial ovarian cancer undergoing a two-step surgical management protocol from January 2010 to April 2019 at Institut Claudius Regaud, a French comprehensive cancer center. The study included patients who underwent upfront or interval cytoreduction after three to four cycles of neoadjuvant platinum and taxane-based chemotherapy. Patients were eligible when CRS was performed during the weeks following staging laparoscopy (two-step surgical management protocol), when they were selected for complete cytoreduction after diagnostic laparoscopy, and when PCI score was recorded during both laparoscopy and laparotomy. Patients were excluded when diagnostic laparoscopy and CRS were performed the same day, and when patients treated with neoadjuvant chemotherapy did not undergo a diagnostic laparoscopy the weeks before interval debulking surgery. Institutional Review Board approval was obtained from our center.
Surgery
All patients underwent a laparoscopic staging to evaluate the extent and distribution of peritoneal carcinomatosis throughout the 13 abdominopelvic regions with PCI, this score was calculated by the senior surgeon [12].
Neoadjuvant chemotherapy was indicated in selected patients who were unfit to withstand multivisceral resection due to medical co-morbidities or poor performance status, in case of non-resectable disease, or in case of needing a too extensive surgery to achieve complete cytoreduction.
Criteria of non-resectability according our center philosophy are deep infiltration of the small bowel mesentery, diffuse carcinomatosis involving large parts of the small bowel or the stomach, infiltration of the duodenum or the pancreas (not limited to the pancreatic tail), or more than two bowel resections required to eradicate the disease.
Candidates for complete CRS were scheduled the following weeks after staging laparoscopy depending on our operating room waiting list and on the preoperative evaluation of the patient. PCI was calculated by the senior surgeon after concluding the tumor debulking surgery [12]. Cytoreductive and peritonectomy procedures were performed following Sugarbaker principles of peritonectomy [13]. Residual disease was assessed using the Completeness Cytoreduction score (CC-0: no residual tumor; CC-1: residual disease less than 2.5 mm in diameter; CC-2: residual nodules between 2.5 mm and 2.5 cm; and CC-3 residual nodules greater than 2.5 cm or a confluence of unresectable disease) [12]. Both surgical procedures were performed or supervised by one of the two experienced oncological surgeons (AM, GF) of our team. We used Aletti Score to quantify the surgical complexity [14]. A surgery was considered ultraradical when at least two of the following procedures were performed: small or large bowel resection, splenectomy, atypical hepatic resection, cholecystectomy, partial gastrectomy, distal pancreatectomy and celiac lymph node dissection [15].
Study data
Medical database was carefully examined to collect all relevant information. Patient demographic data, cancer antigen-125 (CA-125) dosage, presence of ascites, neoadjuvant chemotherapy, PCI scores recorded during both staging laparoscopy and laparotomy [12], surgical procedures performed during CRS, surgical complexity according to Aletti score, operative time, fluid loss, localization of residual disease, and histologic data were retrieved from our database.
Statistical analysis
Data were summarized by frequencies and percentages for categorical variables and by medians and interquartile ranges (IQR) for continuous variables. PCI score was considered as a continuous variable, and concordance between laparoscopic and laparotomic values was evaluated using intraclass correlation coefficient (ICC) with a one-way random effects model and interpreted following Cicchetti and Domenic guidelines [16]. Concordance was also visually assessed using Bland–Altman plots of the average against the differences of the measurements. Non-parametrical Wilcoxon matched-pairs signed-rank test was used to compare the differences in PCI assessed by both types of surgical approaches and to estimate the 95% confidence intervals (95% CI).
The influence of different factors over laparoscopic PCI’s capacity to predict the true value given by laparotomic evaluation was assessed using simple and stepwise linear regression analysis, while logistic regression was used to determine its capacity to predict complete cytoreduction (CC-0), expressed as odds ratio (OR) with its 95% CI. The receiver-operating characteristics (ROC) curve was plotted. Laparoscopic PCI’s capacity to predict CC-0 was assessed using the area under the curve (AUC).
Finally, in patients in whom all expected surgical procedures could be carried out (CC-0 and CC-1), Fisher’s exact test was used to evaluate the association between laparoscopic PCI score (in two categories, if PCI was equal or above zero) with the surgery performed at each region of interest. For this purpose, only not-standard procedures performed in the treatment of peritoneal carcinomatosis were considered; hysterectomy, bilateral adnexectomy and infragastric omentectomy were standard procedures and, therefore, were excluded.
p values below 0.05 were considered statistically significant. All statistical analyses were conducted using STATA 13.0 (StataCorp, Texas, USA).
Results
During the study period, 543 patients underwent a staging laparoscopy for possible ovarian carcinomatosis. Among them, 43 patients fulfilled the inclusion criteria. Clinical characteristics and surgical data are listed in Table 1. All patients were in a good performance status. Neoadjuvant chemotherapy was administered in 21% of patients. The median PCI during staging laparoscopy was 11 (IQR 7–16), and the median PCI found during CRS was 17 (IQR 10–23). The median number of affected areas in laparoscopic PCI was 7 (IQR 4–10), and the median number of affected areas in laparotomic PCI was 10 (IQR 5–12). The median delay between both surgeries was 14 days (IQR 10–27). In one patient, the delay was 42 days, because in positron emission tomography combined with computed tomography (PET/CT) an intraluminal rectal lesion was found, and a coloscopy with biopsies was performed before CRS. This lesion finally corresponded to a villous adenoma. In another case, CRS was scheduled 49 days after diagnostic laparoscopy on request of the patient due to personal issues.
The ICC between laparoscopic and laparotomic PCI was 0.54 (95% CI 0.29–0.72), which is considered a fair correlation [16]. The association, in presence of all possible confounders, was also evaluated using stepwise linear regression analysis, whose results are summarized in Table 2. The time between surgeries significantly increased the difference between both PCI assessments (Fig. 1). Neoadjuvant chemotherapy, body mass index, and history of previous abdominal surgery were not significantly associated with PCI score difference between laparoscopy and laparotomy. For an initial difference between both PCI scores of 2.07, laparotomic PCI is increased by 0.96 units (95% CI 0.71–1.21) for each point of laparoscopic PCI, and by 0.20 units (95% CI 0.07–0.33) for each day that passed between laparoscopy and laparotomy. When laparoscopic PCI was modified using the rounded coefficients of the linear regression equation: laparoscopic PCI + 0.2x[days between surgeries] + 2, the ICC between modified laparoscopic PCI and laparotomic PCI increased to 0.79 (95% CI 0.65–0.88), which can be classified as excellent [16]. To illustrate the application of the equation, a woman who presents a laparoscopic PCI of 6, if the CRS is scheduled 15 days later, the expected PCI during this surgery is 11 (6 + 0.2 × 15 + 2).
Bland–Altman plots showed that after applying the abovementioned equation, the mean difference was no longer statistically different from zero (5.16, p < 0.001 vs. − 0.34, p = 0.27) and the distribution of values strengthened around this estimate (Fig. 2).
Bland–Altman plots showing the variability of Peritoneal Cancer Index (PCI) determination through laparoscopic and laparotomic evaluation. The graph on the left illustrates the differences between the values observed during each surgery (a), while the plot on the right displays the difference of the laparotomic value with modified-laparoscopic value after applying the regression equation (b). These graphs illustrate that, when comparing laparotomic PCI value with the modified laparoscopic score, the distribution of differences narrows around their mean, which, in turn, gets closer to zero
When considering separately every PCI region, the best concordance was found in region A6 (ICC 0.70), where the mean PCI difference between both approaches was not statistically significant (Table 3).
Completeness cytoreduction score and laparoscopic PCI were significantly associated (OR 1.27, 95% CI 1.03–1.57, p = 0.03). For this analysis, one patient was excluded. She was considered completely resectable, but she presented an intraoperative anaphylaxis shock with maintained hypotension and surgery was abandoned (considered as CC-2). Among the 42 patients included for this analysis, 38 patients (90.5%, 38/42) underwent a complete cytoreduction (CC-0) and had a median laparoscopic PCI of 11 (IQR 7–14). The 4 patients (9.5%, 4/42) with residual disease had a median laparoscopic PCI score of 19 (IQR 17.5–21). Among these 4 patients, surgery was abandoned in two cases before starting cytoreduction due to the need of multivisceral procedures with more than two bowel resections to achieve CC-0 in one case and due to a massive retraction of the mesentery in the other case. Both cases were considered CC-3. In a third patient, a CRS was started but a massive pleural invasion -discovered during the right diaphragmatic peritonectomy-precluded a complete cytoreduction and the surgery was abandoned (also considered as CC-3). Finally, the last patient remained with minimal millimetric disease in the bowel after CRS (considered CC-1). The ROC curve for the ability of laparoscopic PCI to predict a complete cytoreduction was plotted, with an AUC of 0.90 (95% CI 0.80–1.00).
Table 4 shows the association between categorized laparoscopic PCI scores and the need of a non-standard surgical procedure for each PCI region. PCI laparoscopic assessment successfully identified the requirement of a surgical procedure only in areas A1 and A3. Laparoscopic PCI was not significantly associated with ultraradical surgery (p = 0.26).
Discussion
No visible tumor residue after CRS is the most important prognostic factor for long-term survival in patients with ovarian carcinomatosis [1, 2]. Several reports have focused on patient selection for upfront cytoreduction based on preoperative imaging. However, conventional imaging such as computed tomography (CT) and magnetic resonance imaging are not able to detect ovarian peritoneal carcinomatosis when lesions measure less than 1 cm, underestimating the disease, and, therefore, cannot always be a substitute of surgical staging [17, 18]. Other imaging tools such as positron emission tomography/computed tomography (PET/CT) have been evaluated, showing a high rate of false negative results in ovarian carcinomatosis lesions below 5 mm [19]. Even if imaging staging before CRS is the standard of care in some countries, laparoscopic staging may add valuable information. Laparoscopic assessment has demonstrated to decrease laparotomy-related morbidity surgical complications, blood loss, hospital stay, interruption of diet intake, and delay to chemotherapy in patients non-primary resectable [8, 20]. Objective assessment during staging laparoscopy to standardize the term of resectable disease is needed, to ensure that the results are concordant across different studies. For this reason, some indexes such as PCI score, have been developed [9].
Most centers schedule diagnostic laparoscopy and CRS within the same day, with the disadvantage of wasting a whole surgical time slot in case of non-resectability, which could negatively impact the waiting list for other patients. In our center, we stablished a two-step surgical management protocol, in which staging laparoscopy is quickly performed after carcinomatosis diagnosis and CRS is scheduled within the following weeks depending on our operating room waiting list and on the preoperative evaluation of the patient. Main advantages of this two-step procedure include the possibility of a quick schedule of laparoscopy as well as to avoid the delay of neoadjuvant chemotherapy in non-resectable patients. This protocol also avoids the unnecessary complete preoperative anesthesiologic management for laparotomy with thoracic epidural analgesia and multiple central venous accesses in non-resectable patients. Moreover, the diagnostic laparoscopy allows to have the histological ovarian cancer subtype before cytoreduction and, therefore, to adapt the surgical effort. There are no previous studies assessing the concordance of PCI score between laparoscopy and laparotomy with a two-step protocol.
Concordance evaluation
In our study, laparoscopic PCI underestimated the laparotomic PCI by two points, and every point increased in laparoscopic PCI was traduced by an increased point in laparotomic PCI. Gouy et al. found that laparoscopic PCI underestimated laparotomic PCI score by approximately three points. They also showed high concordance of laparoscopic and laparotomic PCI calculated at the end of CRS between junior and senior surgeons. ICC was 0.69 (95% CI, 0.50–0.88) and 0.64 (95% CI, 0.43–0.86) among senior and junior surgeons, which is higher than concordance observed in our study (ICC 0.54) [11]. However, in this study, PCI scores were calculated by the same surgeon during the same surgical procedure, which could enhance PCI concordance. Our study aimed to evaluate PCI score concordance when a two-step surgical management was proposed. Delay between surgeries and assessment by a different surgeon may explain lower the concordance in our study. Time between surgeries significantly increased the PCI score calculated at CRS, probably due to disease progression. For every 5 days elapsed between laparoscopy and laparotomy, laparotomic PCI increased one point. After applying the linear equation, the ICC was improved to 0.79, which is considered as an excellent concordance [16]. We consider that optimal time to schedule CRS is maximum 10 days after laparoscopic assessment. A delay of 10 days or less to perform CRS would mean an increase in final PCI of maximum 2 points, which would probably not modify resectability. However, the CRS has to be scheduled as soon as possible.
Fagotti et al. developed a different laparoscopic scoring algorithm, referred to as the predictive index value (PIV) [21]. Hansen et al. evaluated concordance between a laparoscopic PIV and extent of ovarian peritoneal carcinomatosis identified at primary CRS. The overall concordance between laparoscopy and laparotomy was high (96%). Concordance varied between anatomic locations, with the lowest and highest concordance seen in bowel infiltration (74.7%) and peritoneal carcinomatosis (94.8%) [22]. In our study, after analyzing separately every PCI area, we reported the best concordance in the pelvis (A6), which is concordant to Hansen et al. study as peritoneal carcinomatosis includes pelvic disease. Another prospective multicentric trial demonstrated that bowel infiltration and mesenteric retraction had the lowest accuracy rate in laparoscopic assessment of peritoneal carcinomatosis, and were non-evaluable in 10% and 25.8% of cases, respectively [23]. In agreement with reported data, our results showed the lowest concordance in the exploration of the small bowel and mesentery. Bowel and mesenteric disease are associated with high tumor abdominal burden that may limit laparoscopic exploration of these regions. Preoperative imaging by CT or PET/CT also have poor sensibility to detect bowel and mesentery disease [18, 24].
Another report evaluated interobserver reproducibility of PCI score. Concordance between PCI score was very high (close to 90%) between senior and junior surgeons before and after CRS for peritoneal carcinomatosis of different origins. After CRS, the mean PCI score increased by approximately two points. Concordance did not depend on the level of the PCI score or on the tumor origin [25]. Underestimation of the PCI score at the beginning of the procedure can be explained by exposure of tumor nodules only visible after visceral mobilization.
Prediction of resectability
Main issue in laparoscopic assessment of peritoneal carcinomatosis is prediction of complete cytoreduction [6,7,8, 26]. A multicentric randomized trial demonstrated that diagnostic laparoscopy significantly reduced the number of futile laparotomies to 10%, as well as the number of patients undergoing multiple laparotomies [8]. In an attempt to improve objective assessment of peritoneal carcinomatosis, several scores have been developed [9, 21].
We found that laparoscopic PCI could predict complete cytoreduction with a good accuracy, and 91% of the patients of our study underwent a complete cytoreduction. Laparoscopic PCI allowed to identify patients requiring a surgical procedure in both right and left upper abdominal quadrant. Several studies have evaluated PCI accuracy to predict complete cytoreduction. Llueca et al. evaluated the ability of PCI assessed by CT, laparoscopy and laparotomy. They found that the best individual method to predict resectability was PCI evaluation by laparotomy. As well, PCI score < 20 assessed by combination of CT and laparoscopy predicted optimal cytoreduction in more than 90% of cases [27]. To date, there is no stablished PCI cutoff to decide whether to perform or not CRS. It is not possible to standardize a PCI score cut-off to withdraw surgical candidates, as surgical effort also depends on other factors such as age and performance status, medical comorbidities, or histologic type and chemosensitivity. Laparoscopic PCI score has been included in several predictive models which have been developed to assess resectability in ovarian carcinomatosis. These models also included other variables such as diaphragmatic carcinomatosis assessed by CT, age, and CA-125 dosage [28, 29]. However, none of these models have been validated and are not used in current clinical practice.
Other authors suggest that selected PCI regions, such as the small intestine (areas 9 to 12) and hepatoduodenal ligament (area 2), were more predictive of residual disease and survival than the entire PCI score. They considered that diagnostic laparoscopy has poor accuracy to explore these areas. Authors proposed early intraoperative examination of these anatomic regions by periumbilical laparotomy, before performing a complete pubic-sternal laparotomy [30]. However, open diagnostic laparotomy increases morbidity and postoperative pain when compared to laparoscopic approach [8, 20]. Our results show excellent concordance between laparoscopic and laparotomic evaluation of PCI Area 2 (ICC 0.80), and lower concordance for the small bowel.
Several studies have showed a good accuracy of PIV to predict resectability [21, 22, 31, 32]. Fagotti-modified score including only 4 of the 7 parameters has also demonstrated a high performance to predict resectability [33]. Chéreau et al. compared the 6 scoring systems to predict resectability in advanced ovarian cancer: International Federation Gynecology and Obstetrics (FIGO), PCI, Eisenkop, Aletti, PIV, and Fagotti-modified scores. They concluded that the most relevant scoring systems for predicting resectability were Fagotti-modified score (AUC 0.76) and PCI (AUC 0.69) [34], in concordance with our results (PCI AUC 0.90). Only the Aletti score remained significant to predict resectability, suggesting that complete resectability is more related to surgical effort than to disease extent [34]. This study has been criticized as the different scoring systems were conceived in different clinical settings and with different aims [34].
To our knowledge, this is the first study presenting a model which allows to calculate the laparotomic PCI with the laparoscopic PCI when performing a two-step surgical protocol. It is the first report assessing laparoscopic and laparotomic PCI concordance by anatomic regions. Main strengths of our study are the prospective data collection, PCI assessment during surgeries, and sample homogeneity. Main limitation is the low number of patients included in the study due to the strict inclusion and exclusion criteria. Less than 10% of the eligible patients (43/543) were finally included in our study, which could have introduced a selection bias. Moreover, it would have been interesting to compare the group of patients undergoing the two-step surgical management with the patients in the one-step surgical protocol. However, in our center, when the laparoscopy and the CRS are performed the same day, the PCI score is only calculated once, and therefore, it is impossible to assess the concordance between laparoscopy and laparotomy. Further prospective studies are necessary to validate the findings reported in this retrospective cohort.
Conclusion
The concordance between laparoscopic PCI assessment and PCI score at the end of CRS is fair when employing a two-step procedure protocol. Laparoscopic assessment underestimates final PCI score by two points, and this difference increases with the delay between both procedures. Diagnostic laparoscopy in a two-step protocol is an adequate procedure to select patients for CRS, with a high accuracy to predict complete cytoreduction. The optimal time to perform CRS is no more than 10 days after staging laparoscopy.
References
Chi DS, Eisenhauer EL, Lang J, Huh J, Haddad L, Abu-Rustum NR, Sonoda Y, Levine DA, Hensley M, Barakat RR (2006) What is the optimal goal of primary cytoreductive surgery for bulky stage IIIC epithelial ovarian carcinoma (EOC)? Gynecol Oncol 103:559–564. https://doi.org/10.1016/j.ygyno.2006.03.051
Bristow RE, Tomacruz RS, Armstrong DK, Trimble EL, Montz FJ (2002) Survival effect of maximal cytoreductive surgery for advanced ovarian carcinoma during the platinum era: a meta-analysis. J Clin Oncol 20:1248–1259. https://doi.org/10.1200/JCO.2002.20.5.1248
Ozols RF, Bundy BN, Greer BE, Fowler JM, Clarke-Pearson D, Burger RA, Mannel RS, DeGeest K, Hartenbach EM, Baergen R, Mackey D (2003) Phase III trial of carboplatin and paclitaxel compared with cisplatin and paclitaxel in patients with optimally resected stage III ovarian cancer: a gynecologic oncology group study. J Clin Oncol 21:3194–3200. https://doi.org/10.1200/JCO.2003.02.153
Wright AA, Bohlke K, Armstrong DK, Bookman MA, Cliby WA, Coleman RL, Dizon DS, Kash JJ, Meyer LA, Moore KN, Olawaiye AB, Oldham J, Salani R, Sparacio D, Tew WP, Vergote I, Edelson MI (2016) Neoadjuvant chemotherapy for newly diagnosed, advanced ovarian cancer: society of gynecologic oncology and american society of clinical oncology clinical practice guideline. Gynecol Oncol 143:3–15. https://doi.org/10.1016/j.ygyno.2016.05.022
NCCN, Ovarian Cancer, Humana Press, Totowa, NJ, 2013. https://doi.org/10.1007/978-1-62703-547-7
Brun J-L, Rouzier R, Selle F, Houry S, Uzan S, Daraï E (2009) Neoadjuvant chemotherapy or primary surgery for stage III/IV ovarian cancer: contribution of diagnostic laparoscopy. BMC Cancer 9:171. https://doi.org/10.1186/1471-2407-9-171
Gómez-Hidalgo NR, Martinez-Cannon BA, Nick AM, Lu KH, Sood AK, Coleman RL, Ramirez PT (2015) Predictors of optimal cytoreduction in patients with newly diagnosed advanced-stage epithelial ovarian cancer: Time to incorporate laparoscopic assessment into the standard of care. Gynecol Oncol 137:553–558. https://doi.org/10.1016/j.ygyno.2015.03.049
Rutten MJ, Van Meurs HS, Van De Vrie R, Naaktgeboren CA, Fons G, Opmeer BC, Spijkerboer A, Bossuyt PMM, Kenter GG, Buist MR, Gaarenstroom KN, Van Gorp T, Brugge HGT, Hofhuis W, Schreuder HWR, Van Haaften M, Arts HJG, Zusterzeel PLM, Pijnenborg JMA, Vos MC, Engelen MJA, Boss EA, Gerestein KG, Schutter EMJ, Mol BW (2017) Laparoscopy to predict the result of primary cytoreductive surgery in patients with advanced ovarian cancer: a randomized controlled trial. J Clin Oncol 35:613–621. https://doi.org/10.1200/JCO.2016.69.2962
Sugarbaker PH (1998) Intraperitoneal chemotherapy and cytoreductive surgery for the prevention and treatment of peritoneal carcinomatosis and sarcomatosis. Semin Surg Oncol 14:254–261
Tentes A-AK, Tripsiannis G, Markakidis SK, Karanikiotis CN, Tzegas G, Georgiadis G, Avgidou K (2003) Peritoneal cancer index: a prognostic indicator of survival in advanced ovarian cancer. Eur J Surg Oncol 29:69–73
Gouy S, Belghiti J, Uzan C, Canlorbe G, Gauthier T, Morice P (2013) Accuracy and reproducibility of the peritoneal cancer index in advanced ovarian cancer during laparoscopy and laparotomy. Int J Gynecol Cancer 23:1699–1703. https://doi.org/10.1097/IGC.0b013e3182a616a7
Gilly FN, Cotte E, Brigand C, Monneuse O, Beaujard AC, Freyer G, Glehen O (2006) Quantitative prognostic indices in peritoneal carcinomatosis. Eur J Surg Oncol 32:597–601. https://doi.org/10.1016/j.ejso.2006.03.002
Sugarbaker PH (1995) Peritonectomy procedures. Ann Surg 221:29–42. https://doi.org/10.1097/00000658-199501000-00004
Aletti GD, Santillan A, Eisenhauer EL, Hu J, Aletti G, Podratz KC, Bristow RE, Chi DS, Cliby WA (2007) A new frontier for quality of care in gynecologic oncology surgery: multi-institutional assessment of short-term outcomes for ovarian cancer using a risk-adjusted model. Gynecol Oncol 107:99–106. https://doi.org/10.1016/j.ygyno.2007.05.032
Martinez A, Ngo C, Leblanc E, Gouy S, Luyckx M, Darai E, Classe JM, Guyon F, Pomel C, Ferron G, Filleron T, Querleu D (2016) Surgical complexity impact on survival after complete cytoreductive surgery for advanced ovarian cancer. Ann Surg Oncol 23:2515–2521. https://doi.org/10.1245/s10434-015-5069-z
Cicchetti DV (1994) Interreliability Standards in Psychological Evaluations. Psychol Assess: 284–290
Bailly C, Bailly-Glatre A, Alfidja A, Vincent C, Dauplat J, Pomel C (2009) Peritoneal carcinosis in ovarian cancer: conventional imaging (CT-scan and MRI). Bull Cancer 96:1155–1162
Axtell AE, Lee MH, Bristow RE, Dowdy SC, Cliby WA, Raman S, Weaver JP, Gabbay M, Ngo M, Lentz S, Cass I, Li AJ, Karlan BY, Holschneider CH (2007) Multi-institutional reciprocal validation study of computed tomography predictors of suboptimal primary cytoreduction in patients with advanced ovarian cancer. J Clin Oncol 25:384–389. https://doi.org/10.1200/JCO.2006.07.7800
De Iaco P, Musto A, Orazi L, Zamagni C, Rosati M, Allegri V, Cacciari N, Al-Nahhas A, Rubello D, Venturoli S, Fanti S (2011) FDG-PET/CT in advanced ovarian cancer staging: Value and pitfalls in detecting lesions in different abdominal and pelvic quadrants compared with laparoscopy. Eur J Radiol 80:e98–e103. https://doi.org/10.1016/j.ejrad.2010.07.013
Lee M, Kim WS, Paek J, Lee HS, Yim WG, Kim HJ, Kim WJ, Kim TY, Nam JE (2011) Comparisons of surgical outcomes, complications, and costs between laparotomy and laparoscopy in early-stage ovarian cancer. Int J Gynecol Cancer 21:251–256. https://doi.org/10.1097/IGC.0b013e318208c71c
Fagotti A, Ferrandina G, Fanfani F, Ercoli A, Lorusso D, Rossi M, Scambia G (2006) A laparoscopy-based score to predict surgical outcome in patients with advanced ovarian carcinoma : a pilot study. Ann Surg Oncol 13:1156–1161. https://doi.org/10.1245/ASO.2006.08.021
Hansen JM, Sood AK, Coleman RL, Westin SN, Soliman PT, Ramirez PT, Fellman BM, Schmeler KM, Fleming ND (2018) Concordance of a laparoscopic scoring algorithm with primary surgery findings in advanced stage ovarian cancer. Gynecol Oncol 151:428–432. https://doi.org/10.1016/j.ygyno.2018.10.017
Nick AM, Coleman RL, Ramirez PT, Sood AK (2015) A Framework for personalized surgical approach to ovarian cancer. Nat Rev Clin Oncol 12:239–245. https://doi.org/10.1038/nrclinonc.2015.26
Bristow RE, Duska LR, Lambrou NC, Fishman EK, Neill MJO, Trimble EL, Montz FJ (2000) A model for predicting surgical outcome in patients with advanced ovarian carcinoma using computed tomography:1532–1540.
Elias D, Souadka A, Fayard F, Mauguen A, Dumont F, Honore C, Goere D (2012) Variation in the peritoneal cancer index scores between surgeons and according to when they are determined (before or after cytoreductive surgery). Eur J Surg Oncol 38:503–508. https://doi.org/10.1016/j.ejso.2012.01.001
Rutten MJ, Leeflang MM, Kenter GG, Mol BWJ, Buist M (2014) Laparoscopy for diagnosing resectability of disease in patients with advanced ovarian cancer. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD009786.pub2
Llueca A, Serra A, Rivadulla I, Gomez L, Escrig J, Játiva-Porcar R, Moreno-Clarí E, Montañés-Pauls B, Bellver M, Maiocchi K, Medina-Medina C, Delgado-Barriga K, Rodrigo-Aliaga M, Ruiz N, Herrero C, Maazouzi Y, Piquer D, Segarra B, Del Moral R (2018) Prediction of suboptimal cytoreductive surgery in patients with advanced ovarian cancer based on preoperative and intraoperative determination of the peritoneal carcinomatosis index. Surg Oncol World J. https://doi.org/10.1186/s12957-018-1339-0
Dessapt AL, Huchon C, Ngo C, Bats AS, Bensaid C, Lecuru F (2016) Is complete cytoreductive surgery feasible in this patient with ovarian cancer? Surg Oncol 25:326–331. https://doi.org/10.1016/j.suronc.2016.07.001
Ghisoni E, Katsaros D, Maggiorotto F, Aglietta M, Vaira M, De Simone M, Mittica G, Giannone G, Robella M, Genta S, Lucchino F, Marocco F, Borella F, Valabrega G, Ponzone R (2018) A predictive score for optimal cytoreduction at interval debulking surgery in epithelial ovarian cancer: a two- centers experience. J Ovarian Res. https://doi.org/10.1186/s13048-018-0415-y
Rosendahl M, Harter P, Bjørn SF, Høgdall C (2018) Specific regions, rather than the entire peritoneal carcinosis index, are predictive of complete resection and survival in advanced epithelial ovarian cancer. Int J Gynecol Cancer 28:316–322. https://doi.org/10.1097/IGC.0000000000001173
Fagotti A, Ferrandina G, Fanfani F, Garganese G, Vizzielli G, Carone V, Salerno MG, Scambia G (2008) Prospective validation of a laparoscopic predictive model for optimal cytoreduction in advanced ovarian carcinoma. Am J Obstet Gynecol 199:642.e1-642.e6. https://doi.org/10.1016/j.ajog.2008.06.052
Fagotti A, Vizzielli G, De Iaco P, Surico D, Buda A, Mandato VD, Petruzzelli F, Ghezzi F, Garzarelli S, Mereu L, Viganò R, Tateo S, Fanfani F, Scambia G (2013) A multicentric trial (Olympia–MITO 13) on the accuracy of laparoscopy to assess peritoneal spread in ovarian cancer. Am J Obstet Gynecol 209:462.e1-462.e11. https://doi.org/10.1016/j.ajog.2013.07.016
Brun J-L, Rouzier R, Uzan S, Daraï E (2008) External validation of a laparoscopic-based score to evaluate resectability of advanced ovarian cancers: Clues for a simplified score. Gynecol Oncol 110:354–359. https://doi.org/10.1016/j.ygyno.2008.04.042
Chéreau E, Ballester M, Selle F, Cortez A, Daraï E, Rouzier R (2010) Comparison of peritoneal carcinomatosis scoring methods in predicting resectability and prognosis in advanced ovarian cancer. Am J Obstet Gynecol 202:178.e1-178.e10. https://doi.org/10.1016/j.ajog.2009.10.856
Acknowledgements
The project that gave rise to these results received the support of a fellowship from ”la Caixa” Foundation (ID 100010434). The fellowship code is LCF/BQ/EU18/11650038.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Angeles, M.A., Migliorelli, F., Del, M. et al. Concordance of laparoscopic and laparotomic peritoneal cancer index using a two-step surgical protocol to select patients for cytoreductive surgery in advanced ovarian cancer. Arch Gynecol Obstet 303, 1295–1304 (2021). https://doi.org/10.1007/s00404-020-05874-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05874-y